Chronic Obstructive Pulmonary Disease, commonly known as COPD, is a progressive lung disease that makes it difficult to breathe. “Progressive” means the condition gradually worsens over time. It is a major cause of illness and death worldwide, but it is also largely preventable and manageable. Understanding COPD is the first step toward taking control of your lung health.
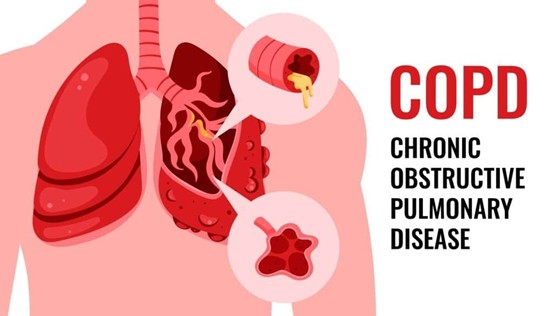
What is COPD? A Closer Look at the Lungs
To understand COPD, it helps to know how your lungs work. When you breathe in, air travels down your windpipe (trachea) into tubes called bronchi, which branch out into smaller tubes (bronchioles) throughout your lungs. At the end of these tubes are tiny air sacs called alveoli. These sacs are elastic and act like balloons, filling with oxygen and then deflating to release carbon dioxide.
COPD is an umbrella term that primarily includes two main conditions, which often occur together:
Emphysema: The walls of the alveoli are damaged and destroyed. This reduces the surface area for gas exchange and causes the lungs to lose their elasticity. The air gets trapped in the damaged sacs, making it hard to exhale fully.
Chronic Bronchitis: This involves a long-term inflammation of the bronchial tubes’ lining. This leads to a persistent, productive cough (producing phlegm) for at least three months a year for two consecutive years. The inflamed airways become swollen and clogged with mucus.
In both cases, the result is an obstruction to the airflow out of the lungs, leading to the characteristic shortness of breath.
Causes and Risk Factors
The primary cause of COPD is long-term exposure to lung irritants that damage the lungs. The most significant risk factor is:
Tobacco Smoking: This is the number one cause, accounting for the vast majority of cases. This includes cigarettes, cigars, pipes, and secondhand smoke.
However, non-smokers can also develop COPD. Other major risk factors include:
Occupational Exposure: Long-term exposure to chemical fumes, vapors, dust, and other harmful substances in the workplace (e.g., in mining, textiles, or construction).
Indoor and Outdoor Air Pollution: In many parts of the world, burning biomass fuels (like wood, crop waste, or coal) for cooking and heating in poorly ventilated homes is a major cause. Heavy outdoor air pollution also contributes.
Genetics: A rare genetic disorder called Alpha-1 Antitrypsin Deficiency can cause COPD, even in non-smokers. This protein protects the lungs, and without it, the lungs are more susceptible to damage.
Recognizing the Symptoms
COPD symptoms are often mild at first but become more severe as the disease progresses. Many people initially dismiss them as signs of aging or being out of shape.Common symptoms include:
Persistent Cough: A chronic cough that doesn’t go away, often called a “smoker’s cough.”
Increased Mucus Production: Frequently coughing up sputum (phlegm).
Shortness of Breath (Dyspnea): This is the hallmark symptom. It may initially occur only during physical activity but can later happen even while at rest. People often describe it as “not being able to get enough air.”
Wheezing: A whistling or squeaky sound when you breathe.
Chest Tightness: A feeling of constriction or pressure in the chest.
A key feature of COPD is “exacerbations,” which are episodes where symptoms suddenly become much worse and last for several days. These are often triggered by a respiratory infection (like a cold or the flu) or air pollution. Exacerbations can be serious, requiring hospitalization, and can accelerate the progression of the disease.
Diagnosis and Treatment
If you experience these symptoms, especially if you are a smoker or have a history of exposure to lung irritants, it is crucial to see a doctor.
Diagnosis typically involves:
Spirometry: This is the most common lung function test. You blow hard into a tube connected to a machine, which measures how much air you can exhale and how fast you can do it.
Chest X-ray or CT Scan: These imaging tests can reveal emphysema and rule out other lung problems.
While there is no cure for COPD, treatments can relieve symptoms, slow disease progression, and improve quality of life.
1. Lifestyle Changes:
Quit Smoking: This is the single most important step.
Avoid Lung Irritants: Stay away from secondhand smoke, pollution, and chemical fumes.
2. Medications:
Bronchodilators: These are inhaled medications that relax the muscles around the airways, helping to open them and make breathing easier. They are usually taken daily with an inhaler.
Inhaled Corticosteroids: These can help reduce inflammation in the airways and prevent exacerbations.
Combination Inhalers: These contain both a bronchodilator and a steroid.
3. Pulmonary Rehabilitation:
This is a personalized program that includes exercise training, nutrition advice, and education about your disease. It teaches you how to manage your condition effectively and stay as active as possible.
4. Oxygen Therapy:
For those with severe COPD and low blood oxygen levels, using supplemental oxygen at home can help improve survival, reduce complications, and increase energy.
5. Vaccinations:
Annual flu shots and the pneumococcal vaccine are essential to prevent respiratory infections that can cause serious exacerbations.
6. Surgery:
In very select cases of severe emphysema, surgical options like lung volume reduction surgery or a lung transplant may be considered.
Prevention is Key
The best way to prevent COPD is to never start smoking or to quit if you already do. Additionally, minimizing exposure to occupational dust and chemicals (using protective equipment) and reducing exposure to indoor air pollution by using clean cooking stoves and ensuring proper ventilation are critical public health measures.
Conclusion
COPD is a serious but manageable disease. Early diagnosis and proactive management are crucial. By understanding the causes, recognizing the symptoms, and adhering to a treatment plan, individuals with COPD can breathe easier, reduce flare-ups, and maintain a better quality of life for years to come. If you are at risk, do not hesitate to speak with your healthcare provider.
Post time: Oct-31-2025