Maintaining healthy blood sugar (glucose) levels is a cornerstone of overall wellness, particularly for individuals with diabetes or prediabetes. Blood sugar monitoring is the essential tool that provides a window into this critical aspect of our metabolism, empowering individuals to make informed decisions about their diet, medication, and lifestyle.
Why Does Glucose Matter?
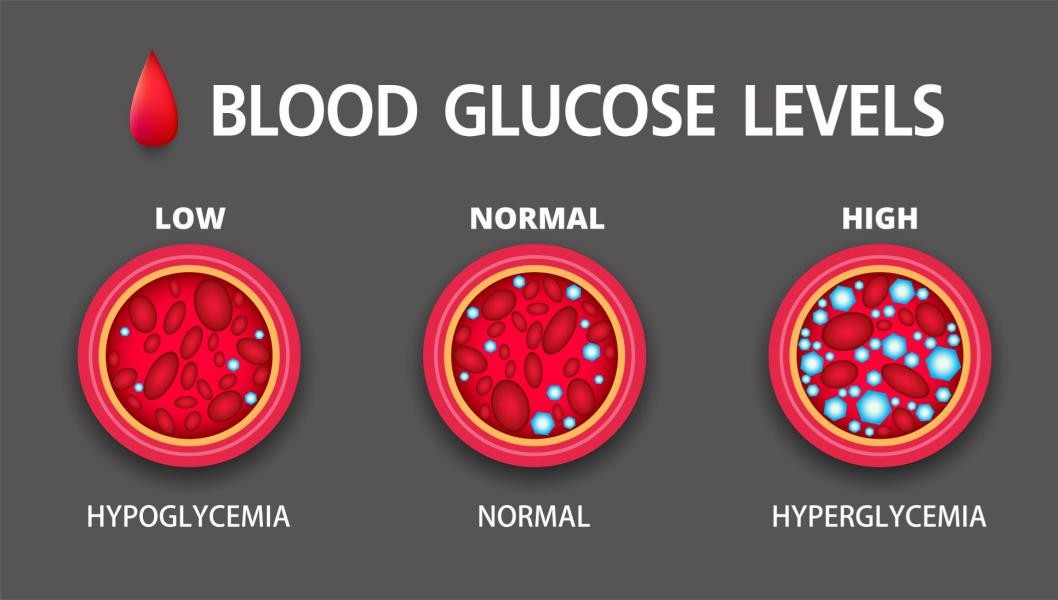
Glucose, derived from the food we eat, is the primary fuel for our body's cells. The hormone insulin, produced by the pancreas, acts as a key, allowing glucose to enter cells and be used for energy. In diabetes, this system is impaired: either the body doesn't produce enough insulin (Type 1) or becomes resistant to its effects (Type 2). This leads to hyperglycemia, or high blood sugar, which, if chronic, can damage blood vessels and nerves, leading to complications affecting the eyes, kidneys, heart, and feet. Conversely, hypoglycemia (low blood sugar), often a risk of diabetes medication, can cause dizziness, confusion, and in severe cases, loss of consciousness.
The Evolution of Monitoring: From Urine to Interstitial Fluid
Historically, glucose monitoring was imprecise, relying on testing urine for the presence of sugar—a delayed and indirect indicator. The revolution began with the invention of the personal blood glucose meter (BGM) in the 1970s. This involves obtaining a small drop of blood via a finger-prick, applying it to a test strip, and inserting it into a meter for a reading. While accurate for a single moment in time, it provides only a snapshot, missing the fluctuations between tests.
The game-changer has been the development of Continuous Glucose Monitors (CGMs). These systems use a tiny sensor inserted just under the skin (usually on the arm or abdomen) to measure glucose levels in the interstitial fluid every few minutes. The data is transmitted wirelessly to a receiver or smartphone, displaying real-time trends, historical patterns, and directional arrows showing whether glucose is rising or falling. This "movie" of glucose levels, as opposed to the "snapshots" from fingersticks, allows for unprecedented insight into how food, exercise, stress, and medication affect an individual's glucose throughout the day and night.
Key Methods and Their Uses
Standard Blood Glucose Meters (BGMs): Remain the most accessible and widely used tool. Essential for calibration of CGMs and for making immediate treatment decisions, especially when CGM readings may be unreliable (e.g., during rapid glucose changes).
Continuous Glucose Monitors (CGMs): Increasingly becoming the standard of care, especially for people on intensive insulin therapy. They are invaluable for identifying trends, preventing highs and lows, and assessing the impact of lifestyle choices. Popular systems include Dexcom G7, Freestyle Libre, and Medtronic Guardian.
Professional CGMs: Worn for a limited period (typically 10-14 days) under a doctor's guidance to collect diagnostic data for therapy adjustment.
For critical health decisions, the direct measurement method of traditional blood glucose meters provides irreplaceable accuracy and reliability. While continuous glucose monitors can display trends, their data is derived from interstitial fluid and has a delay of several minutes. During rapid blood sugar fluctuations or when hypoglycemic symptoms occur, they may fail to reflect the actual blood glucose level. In contrast, traditional blood glucose meters directly analyze capillary blood, delivering immediate and definitive values. They serve as the gold standard for calibrating continuous glucose monitors, adjusting insulin dosage (especially before meals and bedtime), and addressing physical discomfort symptoms. Unaffected by sensor errors, signal interruptions, or calibration issues, traditional meters are also more cost-effective and accessible. They represent the most direct and trustworthy cornerstone for decision-making in diabetes management. Therefore, combining the precise point-of-care testing of traditional blood glucose meters with the dynamic trends from continuous glucose monitoring is the safest and most prudent approach to achieving optimal glycemic control.

Empowerment Through Knowledge
Ultimately, blood sugar monitoring is not an end in itself but a powerful means to an end: achieving better health and preventing complications. By translating numbers into actionable knowledge—understanding which breakfast spikes your glucose or how a walk after dinner helps control it—individuals move from passive patients to active managers of their own health. Whether through traditional fingersticks or advanced continuous sensors, this monitoring is the critical feedback loop that makes effective, personalized diabetes management possible.
The ACCUGENCE ® Multi-Monitoring System can provide four detection methods of blood glucose, meet the test needs of people in diabetic patients. The test method is convenient and fast, and can provide accurate test results, helping you to understand your physical condition in time and obtain better effects of losing weight and treatment.

Post time: Dec-17-2025
