Abstract
Impulse Oscillometry (IOS) is an innovative, non-invasive technique for assessing lung function. Unlike conventional spirometry, which requires forced expiratory maneuvers and significant patient cooperation, IOS measures respiratory impedance during quiet tidal breathing. This makes it particularly valuable for use in children, the elderly, and patients who are unable to perform reliable spirometry. This article reviews the principles, key parameters, clinical applications, advantages, and limitations of IOS in modern respiratory medicine.
Introduction
Pulmonary function tests (PFTs) are essential for diagnosing and managing respiratory diseases. Spirometry, the gold standard, has limitations due to its dependence on patient effort and coordination. Impulse Oscillometry (IOS) has emerged as a powerful alternative and complementary technique that overcomes these challenges by requiring only passive breathing.
Principles of Impulse Oscillometry
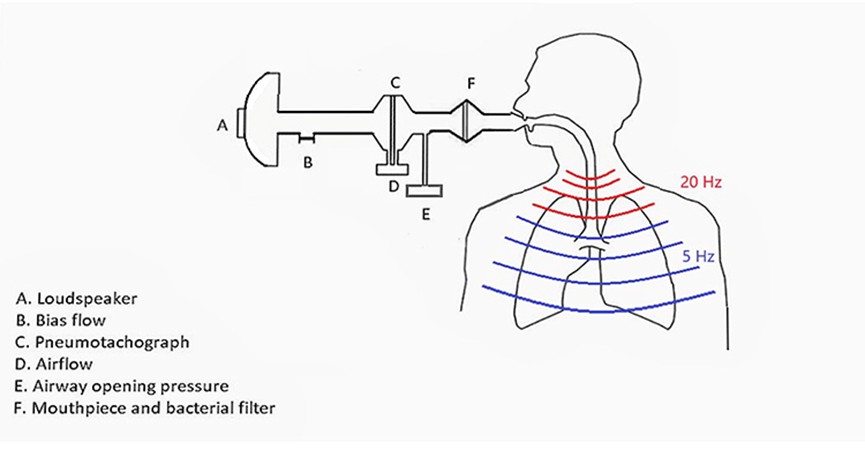
The IOS system applies short, pulsed pressure signals (containing a spectrum of low and high frequencies, typically from 5 to 35 Hz) to the patient’s airways via a mouthpiece. The device simultaneously measures the resulting pressure and flow signals at the mouth. By applying a principle analogous to Ohm’s law in electronics, it calculates Respiratory Impedance (Z).
Respiratory Impedance is composed of two primary components:
Resistance (R): The component of impedance in phase with flow. It primarily reflects the resistive properties of the airways to airflow. Higher frequencies (e.g., 20Hz) penetrate centrally, reflecting central airway resistance, while lower frequencies (e.g., 5Hz) penetrate deeply, reflecting total airway resistance.
Reactance (X): The component of impedance out of phase with flow. It reflects the elastic recoil of the lung tissue and chest wall (capacitance) and the inertial properties of the air in the central airways (inertance).
Key Parameters and Their Clinical Significance
R5: Resistance at 5 Hz, representing total respiratory resistance.
R20: Resistance at 20 Hz, representing central airway resistance.
R5 – R20: The difference between R5 and R20 is a sensitive indicator of peripheral or small airway resistance. An increased value suggests small airway dysfunction.
Fres (Resonant Frequency): The frequency at which reactance is zero. An increase in Fres indicates increased obstruction and stiffness of the lungs, a hallmark of small airway disease.
AX (Reactance Area): The integrated area of reactance from 5 Hz to Fres. An increase in AX is a sensitive marker of peripheral airway impairment.
Forced Oscillation vs. Impulse Oscillation in Lung Function Testing
Both Forced Oscillation Technique (FOT) and Impulse Oscillometry (IOS) are non-invasive methods that measure respiratory impedance during quiet breathing. The key difference lies in the type of signal they use to perturb the respiratory system.
1. Forced Oscillation Technique (FOT)
The Signal: Uses a single, pure frequency or a mixture of predefined frequencies (multi-frequency) simultaneously. This signal is a continuous, sinusoidal wave.
Key Characteristic: It is a steady-state measurement. Because it can use a single frequency, it is very precise for measuring impedance at that specific frequency.
2. Impulse Oscillometry (IOS)
The Signal: Uses very short, pulse-like pressure waves. Each pulse is a square wave that contains a spectrum of many frequencies (typically from 5Hz to 35Hz).
Key Characteristic: It is a transient measurement. A major advantage is that a single pulse provides impedance data across a wide range of frequencies almost instantly.
In summary, while both methods are valuable, IOS’s pulsed technique makes it faster, more patient-friendly, and exceptionally effective at detecting small airway disease, contributing to its widespread clinical adoption.
Advantages of IOS
Minimal Patient Cooperation: Requires only quiet, tidal breathing, making it ideal for young children, the elderly, and critically ill patients.
Comprehensive Assessment: Differentiates between central and peripheral airway obstruction and provides information on lung compliance.
High Sensitivity for Small Airway Disease: Can detect abnormalities in the small airways earlier than spirometry.
Excellent for Monitoring: Allows for repeated and prolonged measurements, useful for bronchial challenge tests, bronchodilator response tests, and monitoring during sleep or anesthesia.
Clinical Applications
Pediatric Pulmonology: The primary application, especially for diagnosing and monitoring asthma in young children.
Asthma: Characterized by elevated R5 and a significant bronchodilator response. IOS is also used to monitor treatment efficacy and detect uncontrolled disease through small airway parameters (R5-R20, AX).
Chronic Obstructive Pulmonary Disease (COPD): Shows elevated resistance and pronounced small airway dysfunction (increased R5-R20, Fres, and AX).
Interstitial Lung Diseases (ILD): Primarily affects reactance, causing a more negative X5 and an elevated Fres, reflecting decreased lung compliance (stiff lungs).
Pre-operative Assessment and Intra-operative Monitoring: Provides a rapid assessment of lung function and can detect acute bronchospasm during surgery.
Evaluation of Unexplained Dyspnea: Helps differentiate between obstructive and restrictive patterns.
Conclusion
Impulse Oscillometry is a sophisticated, patient-friendly technique that has revolutionized pulmonary function testing, particularly in populations where spirometry is challenging. Its ability to detect small airway disease and provide a differentiated analysis of airway mechanics makes it an invaluable tool for the early diagnosis, phenotyping, and long-term management of a wide range of respiratory conditions. While it complements rather than replaces conventional PFTs, IOS has secured a permanent and growing role in the modern respiratory diagnostics arsenal.
Post time: Oct-10-2025