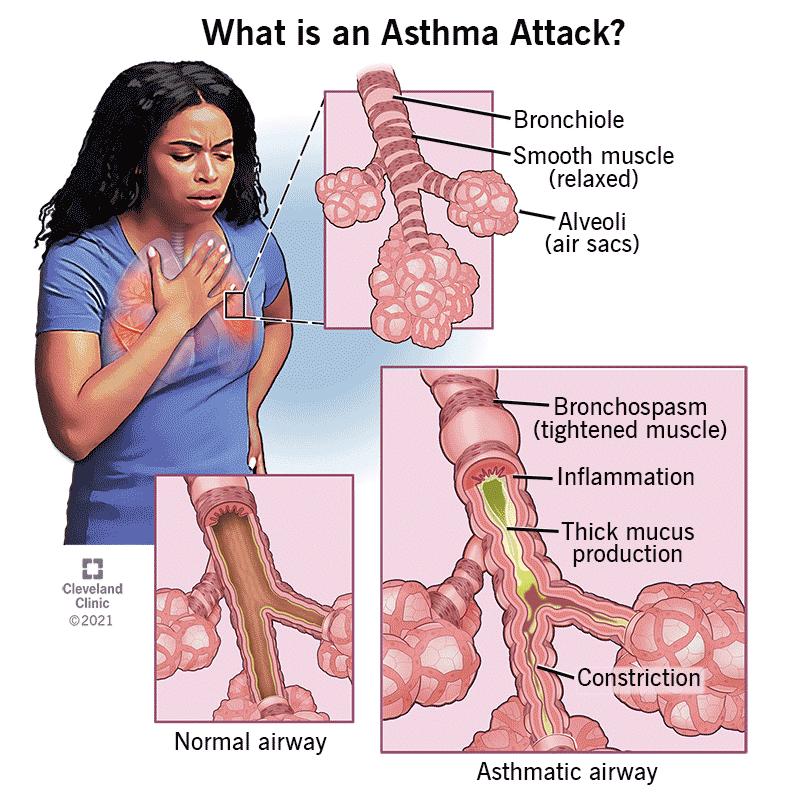
Asthma is a condition that causes long-term (chronic) inflammation in your airways. The inflammation makes them react to certain triggers, like pollen, exercise or cold air. During these attacks, your airways narrow (bronchospasm), swell up and fill with mucus. This makes it hard to breathe or causes you to cough or wheeze. Without treatment, these flare-ups can be fatal.
Millions of people in the U.S. and around the world have asthma. It can start in childhood or develop when you’re an adult. It’s sometimes called bronchial asthma.
Types of asthma include:
Allergic asthma: when allergies trigger asthma symptoms
Cough-variant asthma: when your only asthma symptom is a cough
Exercise-induced asthma: when exercise triggers asthma symptoms
Occupational asthma: when substances you breathe in at work cause you to develop asthma or trigger asthma attacks
Asthma-COPD overlap syndrome (ACOS): when you have both asthma and COPD (chronic obstructive pulmonary disease)
Symptoms and Causes
Symptoms of asthma include:
● Shortness of breath
● Wheezing
● Chest tightness, pain or pressure
● Cough
You might have asthma most of the time (persistent asthma). Or you might feel fine in between asthma attacks (intermittent asthma).
Asthma causes
Experts aren’t sure what causes asthma. But you might be at a higher risk if you:
● Live with allergies or eczema (atopy)
● Were exposed to toxins, fumes or secondhand or thirdhand smoke (residue left behind after smoking), especially early in life
● Have a biological parent with allergies or asthma
● Experienced repeated respiratory infections (like RSV) as a child
Asthma triggers
Asthma triggers are anything that causes asthma symptoms or makes them worse. You might have one specific trigger or many. Common triggers include:
Allergies: pollen, dust mites, pet dander, other airborne allergens
Cold air: especially in winter
Exercise: especially intense physical activity and cold-weather sports
Mold: even if you’re not allergic
Occupational exposures: sawdust, flour, glues, latex, building materials
Respiratory infections: colds, flu and other respiratory illnesses
Smoke: smoking, secondhand smoke, thirdhand smoke
Stress: physical or emotional
Strong chemicals or smells: perfumes, nail polish, household cleaners, air fresheners
Toxins in the air: factory emissions, car exhaust, wildfire smoke
Asthma triggers can bring on an attack right away. Or it might take hours or days for an attack to start after you’re exposure to a trigger.
Diagnosis and Tests
How doctors diagnose asthma? An allergist or pulmonologist diagnoses asthma by asking about your symptoms and performing lung function tests. They’ll ask about your personal and family medical history. It can be helpful to let them know what makes asthma symptoms worse and if anything helps you feel better.
Your provider might determine how well your lungs are working and rule out other conditions with:
Allergy blood tests or skin tests: These can determine if an allergy is triggering your asthma symptoms.
Blood count: Providers can look at eosinophil and immunoglobulin E (IgE) levels and target them for treatment if they’re elevated. Eosinophils and IgE can be elevated in certain types of asthma.
Spirometry: This is a common lung function test that measures how well air flows through your lungs.
Chest X-rays or CT scans: These can help your provider look for causes of your symptoms.
A peak flow meter: This can measure how much your airways are restricted during certain activities.
Management and Treatment
What is the best way to manage asthma? The best way to manage asthma is to avoid any known triggers and use medications to keep your airways open. Your provider might prescribe:
Maintenance inhalers: These usually contain inhaled steroids that reduce inflammation. Sometimes, they’re combined with different types of bronchodilators (medicines that open your airways).
A rescue inhaler: Fast-acting “rescue” inhalers can help during an asthma attack. They contain a bronchodilator that quickly opens your airways, like albuterol.
A nebulizer: Nebulizers spray a fine mist of medication through a mask on your face. You might use a nebulizer instead of an inhaler for some medications.
Leukotriene modifiers: Your provider might prescribe a daily pill to help reduce asthma symptoms and your risk of an asthma attack.
Oral steroids: Your provider might prescribe a short course of oral steroids for a flare-up.
Biologic therapy: Treatments like monoclonal antibodies might help severe asthma.
Bronchial thermoplasty: If other treatments don’t work, your provider may suggest bronchial thermoplasty. In this procedure, a pulmonologist uses heat to thin the muscles around your airways.
Asthma action plan
Your healthcare provider will work with you to develop an asthma action plan. This plan tells you how and when to use your medicines. It also tells you what to do when you have certain symptoms and when to seek emergency care. Ask your healthcare provider to walk you through it.
Post time: Aug-26-2025